Writes Rien D. (L6th)
Walking through the doors of Harefield Hospital, one of the UK’s foremost centres for cardiac and thoracic care, I felt a mixture of excitement and humility. Here, science and compassion combine in life and death decisions every single day. For someone hoping to become a doctor, this school trip offered not just inspiration, but a window into the realities of hospital medicine.
We opened the morning with Dr Vas Paula, who took us deep into the world of heart attacks. He explained by discussing how a myocardial infarction occurs when a coronary artery becomes blocked, often by a clot formed on a ruptured atherosclerotic plaque. He went on to detail how the resultant lack of oxygen rapidly damages heart muscle. He described how early interventions such as primary percutaneous coronary intervention can restore perfusion and limit infarct size. The message was clear; every minute counts. The heart is like a high-performance engine – when fuel (oxygen) is cut off, damage begins.
Next up was Professor William Tof, who challenged us to consider our role in emergencies. He emphasised that as medics, we are not passive onlookers, but potential lifesavers. He presented the harsh truth behind out of hospital cardiac arrests (OHCA) in the UK: fewer than one in twelve patients survive to 30 days. He also outlined how bystander CPR and early defibrillation can dramatically improve survival. His talk made it clear that medical professionals alone cannot solve the problem; it’s a societal responsibility. In short, everyone learning CPR matters.
We then heard from Suzy Brown, a Clinical Nurse Specialist, who offered a fresh perspective on how nursing in the twenty first century is no longer just bedside care. She described how nurses now lead clinics, manage complex technology, participate in decision making, run nurse led pathways and supervise advanced interventions. The profession requires not only clinical skill but critical thinking, leadership and strong communication. Her talk underscored how the entire healthcare team must be highly trained and adaptive.
After a coffee break, Mr Eval Russel gave a fascinating overview of what it takes to run a heart hospital. He explained the balancing act between patient care, staffing, equipment, regulatory compliance and budgeting. He described the tough decisions: allocating funds for new TAVR (transcatheter aortic valve replacement) suites, managing intensive care demand, negotiating with commissioners, all while ensuring quality and safety. It was a reminder that medicine happens in a system, and that clinical knowledge must unite with leadership and resource management.
Later, Dr Rob Smith guided us through heart valve problems and treatments. This is one of the most dynamic areas in cardiology. He then introduced us to the latest TAVR techniques for patients too high risk for open surgery. In these cases, transcatheter implantation offers a less invasive option. This session illustrated the front line of innovation, where technology is improving recovery times for patients who might otherwise be inoperable.
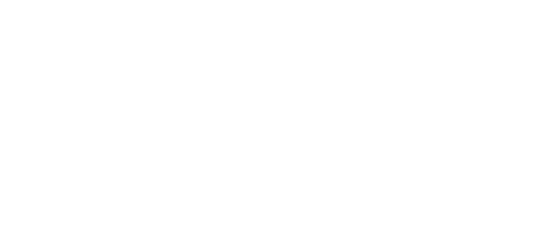
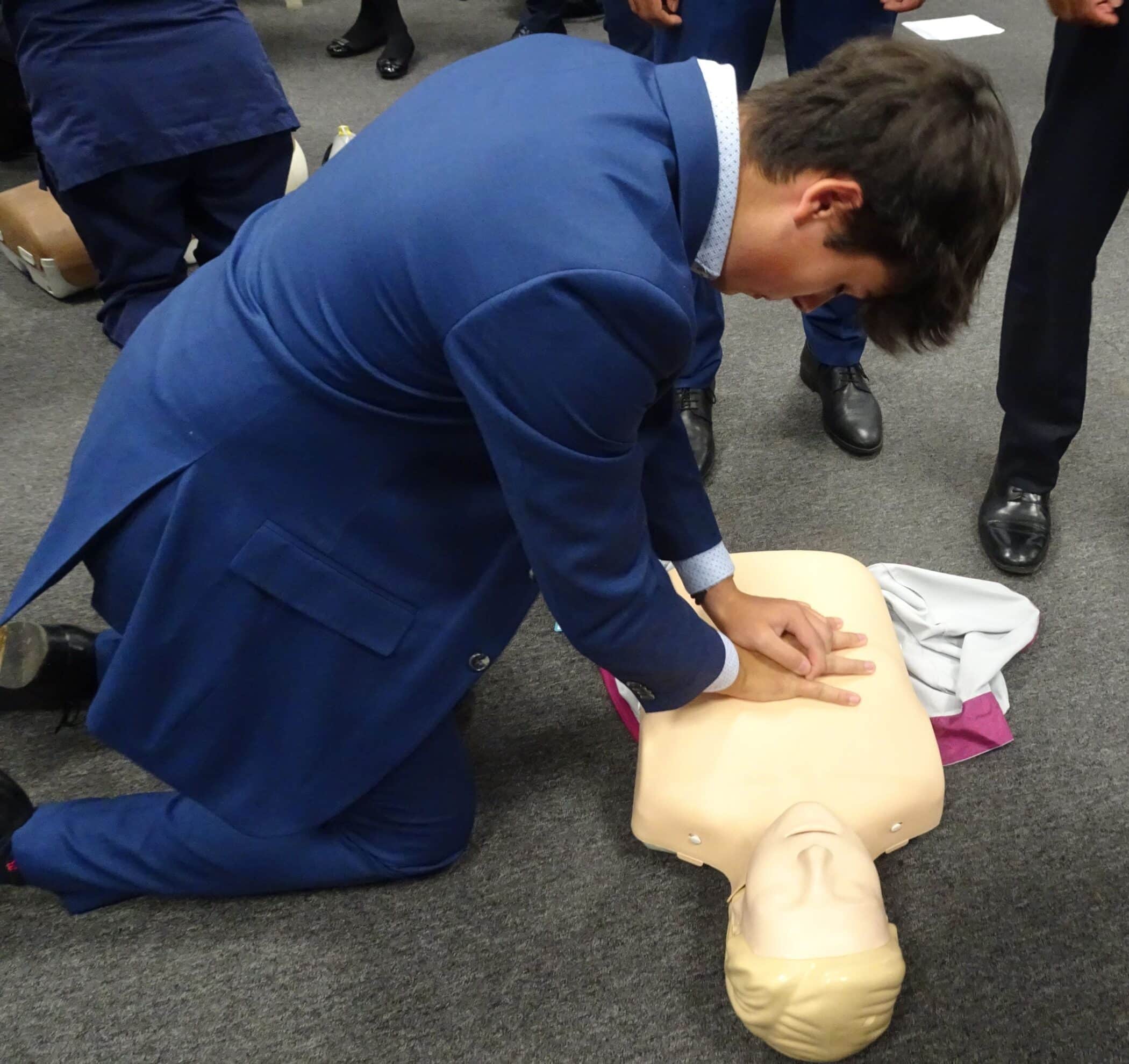
Perhaps most memorable was the hands on session with Alison Pottle and her resuscitation team. They explained each step of CPR, the role of chest compressions, airway management, defibrillation, and how the team coordinates during cardiac arrest. It was exhilarating to experience how high stakes resuscitation really is. It cemented the earlier lectures; that survival often depends not only on knowledge, but on prompt action, training, teamwork and calm under pressure.
In the afternoon we had informal conversations with several doctors – including Dr David Gareth Jones – about the day-to-day reality of being a physician. He spoke openly about medical school stress, long hours, balancing clinical work and research, and the emotional toll of patient loss. He also emphasised the profound rewards: the ability to specialise in niche areas, lead research, and make a tangible difference. He reminded us that even when you can’t cure everything, doing your best with integrity and empathy matters most.